At W Cosmetic Surgery™ in Philadelphia, Dr. Allan Wulc gives each of his patients undivided and individual attention and diagnosis. For patients with thyroid eye disease — also known as Graves’ disease — he performs orbital decompression surgery, eyelid surgery, and cosmetic surgery to help them look and feel more natural and youthful.
What is Thyroid Eye Disease?
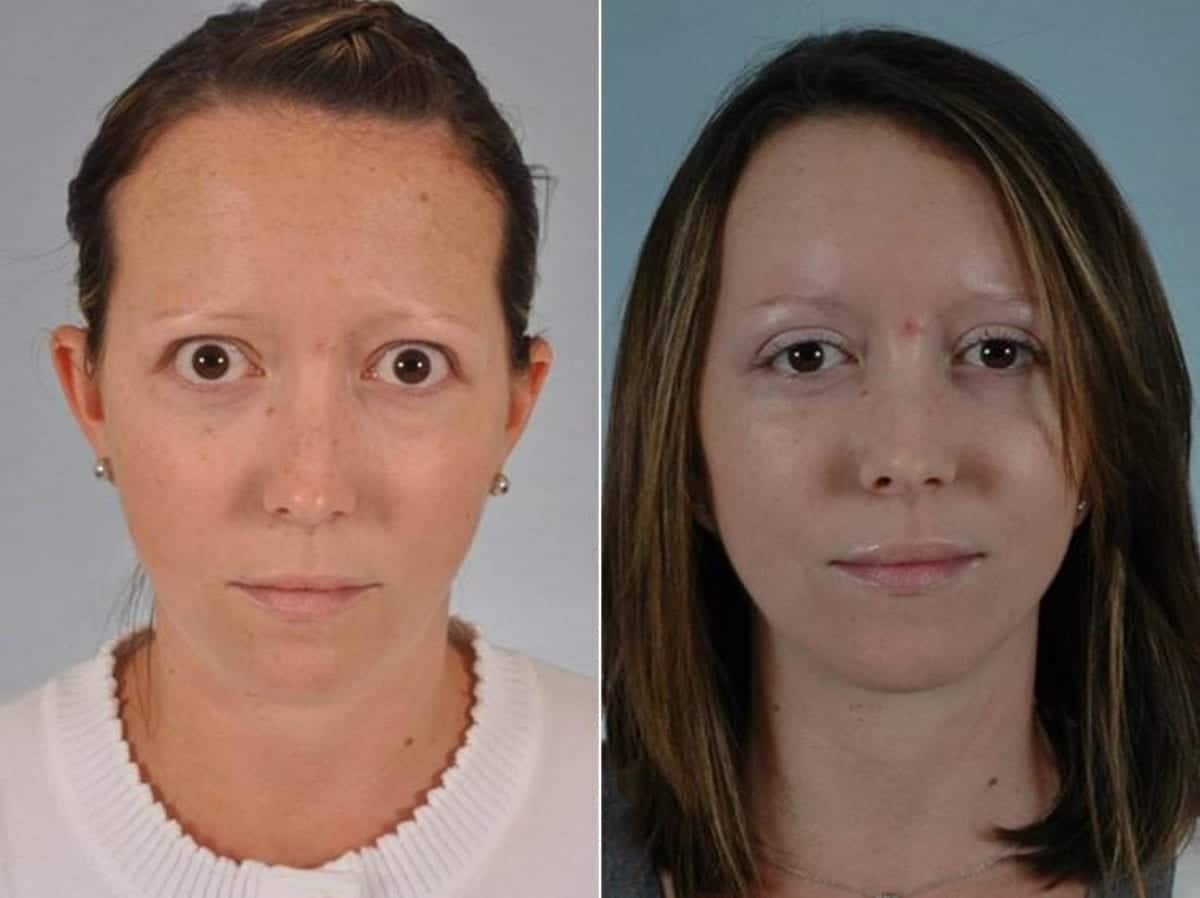
From a cosmetic standpoint, thyroid eye disease — also called Graves’ disease — is a bulging of the eyes and eyelid retraction. This creates a “bug-eye” appearance in patients, which may cause them to look angry, worried, or afraid.
Thyroid eye disease is more prominent in women and can result in blindness, blurred vision, double vision, and general discomfort in the eyes.
GRAVES’ DISEASE EYE SURGERY RESULTS IN PHILADELPHIA
What Treatments are Available for Thyroid Eye Disease?
Treatment for thyroid eye disease is highly individualized. It is based on the severity and presentation of the disease at the time of diagnosis. During your consultation, Dr. Wulc will carefully examine your symptoms to create a customized treatment plan.
Some methods of treatment for thyroid eye disease include:
- Artificial tears and other means of controlling dryness
- Botox® to lower retracted eyelids
- New IV drugs to control swelling, redness, and double vision if steroids have been ineffective
In these cases, we often work cooperatively with the Department of Neurology and Ophthalmology at the University of Pennsylvania or with the neuro-ophthalmologists at Jefferson’s Wills Eye Institute. If radiation is required, we work with radiation specialists at Jefferson and the University of Pennsylvania.
Once disease progression is halted, we give consideration to surgery.
What Will Recovery from Thyroid Eye Disease Surgery Look Like?
In most cases, patients will go home about an hour after the surgery. The surgery is done on an outpatient basis, and for about a week post-operation, ice packs, rest, and topical antibiotic ointment are recommended for a week post-operation. A family member or friend can easily perform these postoperative tasks during your recovery.
For those who are eager to get back to work and play as soon as possible, we have a thoughtfully crafted quick-recover program.
Why Choose W Cosmetic Surgery for your Graves’ Disease Surgery?
We have been performing oculoplastic surgery and have been involved in the care of thyroid eye patients for more than 25 years.
Dr. Wulc is a world-renowned surgeon known for his meticulous and holistic approach to facial cosmetic surgery. He is board-certified in ophthalmology, facial cosmetic surgery, plastic surgery, and a diplomate of the American Society of Ophthalmic Plastic and Reconstructive Surgeons.
Sign Up for a Consultation in Philadelphia
We know how difficult it can be to battle thyroid eye disease. Cosmetic surgery can help you look and feel healthier, younger, and more relaxed. Schedule a consultation with Dr. Wulc at W Cosmetic Surgery, where he’ll give you his undivided attention, advice, and individualized treatment options.
Dr. Wulc looks forward to helping you bring your aesthetic goals to life. Serving customers from Plymouth, Philadelphia, Main Line, PA, and surrounding areas.
Discover your possibilities.
Schedule a consultation
Saturday - Sunday Closed